How OCD and Eating Disorders Often Go Hand in Hand
If you've been struggling with both obsessive thoughts and disordered eating, you're not imagining that there’s a connection.
You might notice intrusive thoughts about food that won't quiet down, rituals around eating that feel impossible to break, or a sense that your brain has hijacked both your relationship with food and your peace of mind.
The exhaustion is real.
The way anxiety shows up in your body, the mental loops that keep you trapped, the feeling that you're failing at recovery because nothing seems to stick.
What often get’s missed is that OCD and eating disorders aren't just happening at the same time by coincidence. They're deeply intertwined, sharing neural pathways and feeding off the same underlying dysregulation in your nervous system.
The Clinical Overlap Between OCD and Eating Disorders
Research shows that obsessive compulsive disorder and eating disorders co-occur at surprisingly high rates. Studies indicate that anywhere from 11% to 69% of people with eating disorders also meet criteria for OCD, depending on the population studied. That's not a small overlap.
Both conditions live in similar neighborhoods of the brain. They both involve:
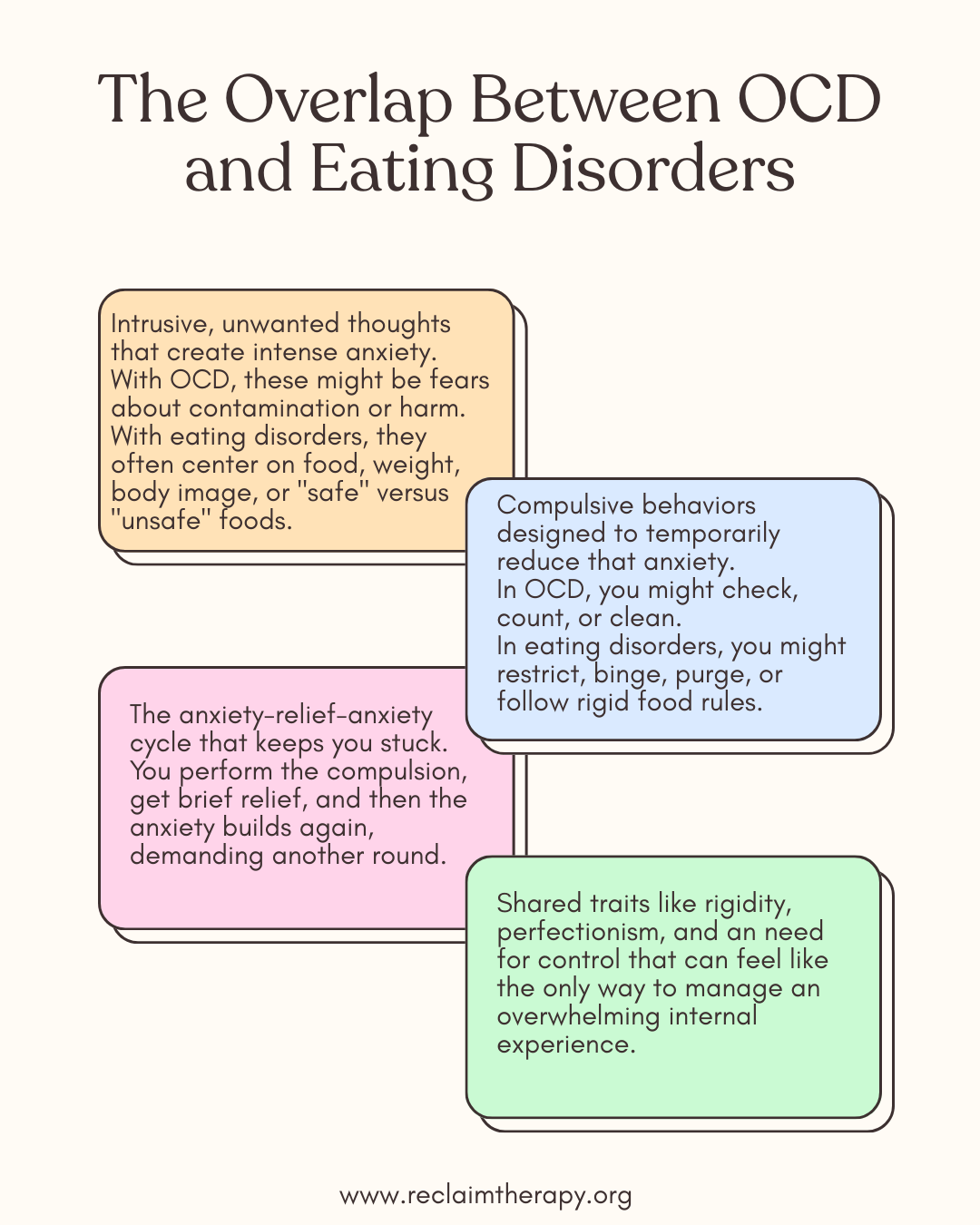
Intrusive, unwanted thoughts that create intense anxiety. With OCD, these might be fears about contamination or harm. With eating disorders, they often center on food, weight, body image, or "safe" versus "unsafe" foods.
Compulsive behaviors designed to temporarily reduce that anxiety. In OCD, you might check, count, or clean. In eating disorders, you might restrict, binge, purge, or follow rigid food rules.
The anxiety-relief-anxiety cycle that keeps you stuck. You perform the compulsion, get brief relief, and then the anxiety builds again, demanding another round.
The overlap is especially prominent in anorexia nervosa. OCD and anorexia share traits like rigidity, perfectionism, and an need for control that can feel like the only way to manage an overwhelming internal experience.
People with OCD and bulimia often describe similar patterns, where bingeing and purging become compulsive responses to intrusive thoughts and anxiety.
Some eating disorders look almost indistinguishable from OCD. Orthorexia, the obsession with "clean" or "healthy" eating, often involves obsessive thoughts about food purity and compulsive behaviors around meal planning and ingredient checking. It sits right at the intersection of both diagnoses.
How to Recognize When Both Are Present
If you're wondering whether this is your story, here are some signs that OCD and eating disorders might be showing up together:
You have ritualistic eating patterns that go beyond preference. Maybe you can only eat foods in a certain order, need to chew a specific number of times, or can't let certain foods touch on your plate. These aren't quirks. They're compulsions that reduce anxiety temporarily.
You experience intrusive thoughts about food that feel impossible to ignore. Thoughts about calories, contamination, or what will happen if you eat certain foods loop in your mind, and eating (or not eating) becomes the compulsion that quiets them.
Fear of contamination extends to food. You might avoid restaurants, won't eat food prepared by others, or have elaborate rules about food safety that go far beyond standard precautions.
You notice perfectionism driving both. There's a "right" way to eat, a "right" weight to be, a "right" way to exercise. Anything less than perfect feels dangerous, and your compulsive behaviors are attempts to hit that impossible standard.
Rumination is constant. You replay meals, analyze food choices, or obsess over your body in ways that feel outside your control. The thoughts aren't just negative. They're sticky, repetitive, and exhausting.
Your anxiety lives in your body. Racing heart before meals, tightness in your chest when you break a food rule, a sense of dread that doesn't match the actual risk of the situation.
Why Trauma Matters in OCD and Eating Disorder Treatment
Here's where (in our opinion!) traditional treatment often misses the mark. Exposure and response prevention (ERP) for OCD and standard eating disorder protocols like meal plans can be helpful, but if there's unresolved trauma underneath, you're essentially asking your nervous system to calm down while it's still in survival mode.
Both OCD and eating disorders are often adaptive responses to overwhelming experiences. Maybe your environment growing up felt chaotic or unsafe, and controlling food or following compulsive rituals became a way to create predictability. Maybe you experienced trauma that left your nervous system stuck in hypervigilance, and obsessive thoughts and disordered eating became strategies to manage the constant sense of threat.
This is especially true for complex trauma.
When your nervous system has learned that the world is dangerous and you can't trust your own body's signals, of course you might develop rigid rules and compulsions. They're not character flaws, they're survival strategies that made sense at the time.
The problem is, those strategies are keeping you stuck now. And, until you address the dysregulation beneath them, you might just keep cycling through the same patterns.
How Reclaim Therapy Treats OCD and Eating Disorders
At Reclaim Therapy, we work with OCD and eating disorders through a trauma-informed lens that gets at the root of both. That means we're not just managing symptoms, we're helping your nervous system heal so the compulsive behaviors and obsessive thoughts lose their grip.
Somatic therapy helps you reconnect with your body's signals. When you've been living in fight-or-flight, your body's cues around hunger, fullness, safety, and danger get scrambled. Somatic Experiencing and other body-based approaches teach you to track sensations, notice when you're dysregulated, and find your way back to regulation without needing the compulsions.
EMDR therapy targets the traumatic memories and beliefs driving both the OCD and the eating disorder. Maybe there's a memory of being criticized about your body, or a moment when food became unsafe, or an experience of losing control that your brain has been trying to prevent ever since. EMDR helps reprocess those memories so they stop triggering the same compulsive responses.
Parts work (Internal Family Systems) recognizes that different parts of you are trying to help in the only ways they know how. One part might be terrified of gaining weight. Another might use food restriction to feel in control. Another might be exhausted and just want relief. Instead of fighting these parts, we help them trust that there are other ways to feel safe. We work with the parts carrying the obsessive thoughts and compulsive eating behaviors, helping them relax their extreme roles.
This approach doesn't just treat the OCD or just treat the eating disorder. It treats the nervous system dysregulation and unresolved trauma that both are stemming from.
When we do that, people often find that both conditions start to soften without the white-knuckle effort that hasn't worked before.
Trauma focused therapy can help with both OCD and Eating Disorder Symptoms
Living with both OCD and eating disorders can feel like you're trapped in a corn-maze with no exit. The obsessive thoughts, the compulsive behaviors, the anxiety that lives in your body. It's exhausting, and it makes sense that you're tired.
What ww know is that these patterns are treatable. When you work with the body, reprocess the trauma, and help the parts of you that are stuck in survival mode, recovery becomes possible. Not the kind of recovery that's about willpower or just pushing through. The kind that actually feels like freedom.
If this resonates, you don't have to figure it out alone. Trauma-focused treatment for OCD and eating disorders can help you get to the root of what's been keeping you stuck.
We’d be happy to support you in your recovery.
🧡,
Getting Help for OCD and Eating Disorders in Montgomery County
If you're in the Philadelphia area and recognize yourself in these patterns, Reclaim Therapy offers specialized treatment for OCD and eating disorders in Horsham, Pennsylvania. Our team of trauma-informed therapists serves clients throughout Montgomery County, Bucks County, the state of Pennsylvania via telehealth and the greater Philadelphia region.
We understand that living with both obsessive compulsive disorder and an eating disorder requires more than surface-level interventions. Our approach using EMDR therapy, Somatic Experiencing, and Internal Family Systems is designed to address the trauma and nervous system dysregulation at the root of both conditions.
Whether you're dealing with OCD and anorexia, OCD and bulimia, or orthorexia with obsessive thought patterns, our therapists in Montgomery County can help you find a path forward that actually addresses what's underneath.
Ready to explore trauma-focused eating disorder treatment?
Contact Reclaim Therapy today to schedule a consultation. We offer both in-person therapy in Horsham, PA and online therapy throughout Pennsylvania.